How Data Performs in APAC Healthcare

Singapore Ministry of Health Director of Data Analytics Sutowo Wong describes some of the ways data makes a difference in healthcare
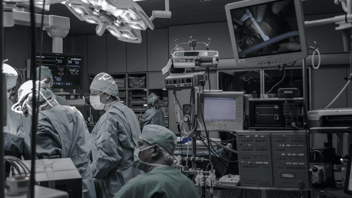
Healthcare, like many industries, is moving to adopt digital and data-driven practices to transform the sector to be more effective, efficient, better connected, and agile.
From patient outcomes to healthcare provider performance and operations, the way data leaders across APAC are applying data science into the fields of healthcare is varied.
Just how varied the field is illustrated well by Sutowo Wong, Director, Data Analytics at the Ministry of Health of Singapore, whose team works on a wide range of data applications across the healthcare space.
“There’s a lot that can be done with data within each domain of health, with use cases ranging from administrative to disease-specific areas,” he says. “One example of a use case in the administrative domain might be simulating the impact on costs as we move from one funding model to another.”
“We also have a methodology to project healthcare expenditure at both a national and government level. We use machine learning to identify outliers in claims for the various health financing schemes that we run.
“Another domain we focus on is infectious diseases, wherein we combine phylogenetics, i.e., analysis of SAR-CoV-2 virus subtypes and epidemiological investigation to identify infection sources and determine how different cases are clustered together.
“When it comes to AI, we use natural language processing to automatically pick up symptoms from free-text physicians’ notes or examine huge data sets. There are many dimensions that can be looked at. For example, to identify spikes in acute respiratory infection (ARI) presentations to hospital emergency departments and Polyclinics.”
Another key use case for data in healthcare is on patient outcomes. Collecting data on how physicians performed and how well patients felt after a procedure is a major area of work for many health-focused data leaders.
In Singapore, Wong says an initiative to collect patient-reported outcome measures has also been introduced.
“Apart from the data that is generated when a patient consumes healthcare services, we can also look at patient-reported outcome measures. Usually, there is a gap in information in between patient visits to healthcare institutions. When they are at home, you don’t really know how they are doing,” he says.
“We have started a process in which we send out surveys to the patients in between visits to understand this more.
“Some of the questions are around understanding, for example, after a surgery, whether the patient has regained some functionality, movement or ability. We’re increasingly looking at things like that.”

Supportive Architecture
Whether it be for frontline clinical applications, operational analytics or administrative systems, data modernisation initiatives are indeed taking place in the APAC region, according to Jon Teo, Regional Healthcare and Data Governance Specialist at the cloud data management software company Informatica.
“We continue to see health analytics activity and data innovation emerging in the region. There is real momentum here,” Teo says. “Covid-19 was certainly an urgent driver of rapid digital adoption, but over the past year we’ve also supported initiatives that were not directly a pandemic response.
“A lot of the work we see reflects a resumption of health systems’ long-term data management strategies, for example establishing cloud or hybrid data platforms, or planting key ‘sources of truth’ to anchor patient analytics, data literacy or regulatory reporting goals.”
Teo adds that establishing architectures that support good data flow, even on the administrative side, can improve the patient experience and efficiency considerably.
“You want to surface the most relevant data about a patient when they make a booking or present themselves at the point of registration, regardless of where that data sits,” he says.
“As some health organisations have embraced cloud-based applications for their administrative needs, having an intelligent data architecture to bridge between on-premises clinical systems and their CMS or patient management processes in the cloud, has made a big difference.”
“Having the right information for a positive patient interaction means having the intelligence to filter out “noise” such as repeatedly rescheduled appointments, as well as link disparate online and offline touchpoints through a reliable patient and provider identifiers. In some cases, we have observed increased patient satisfaction scores, as well as up to a 3-fold increase in appointment volume.”
This article is an excerpt from our Data and Analytics in Healthcare APAC 2022 report. Also, don’t miss your chance to hear directly from Informatica’s Jon Teo at Data & Analytics in Healthcare Online ASEAN.